Chronic Kidney Disease Calcium
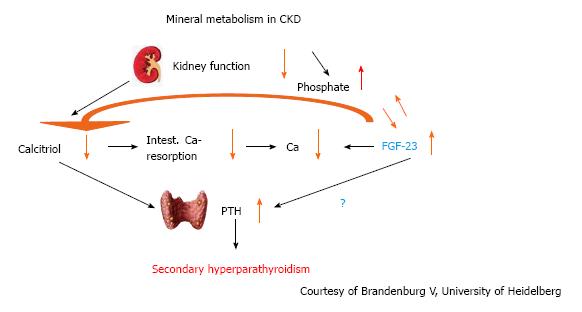
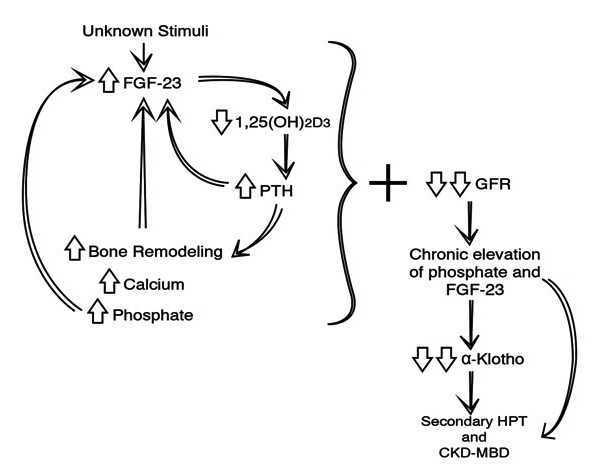
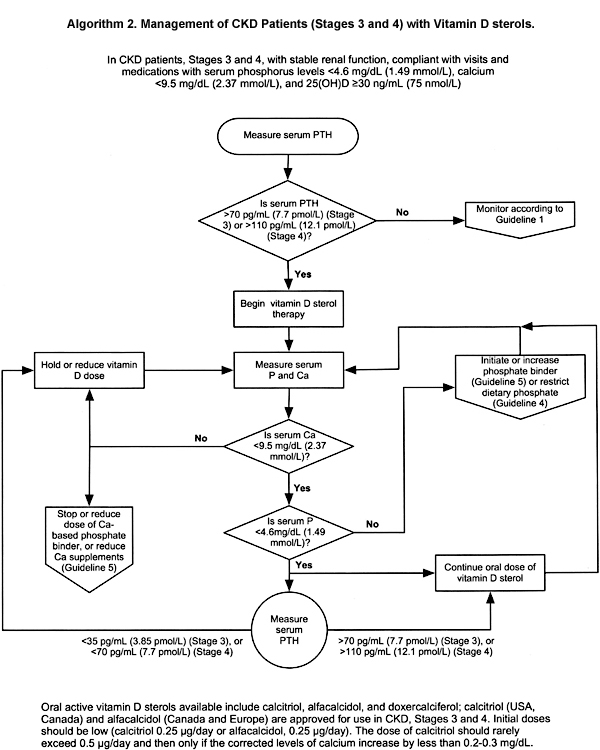
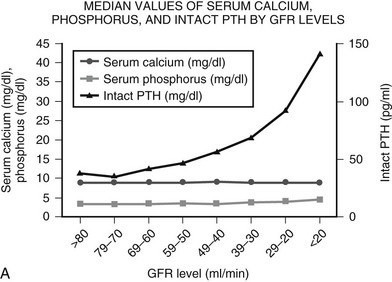
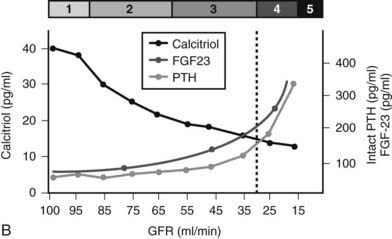
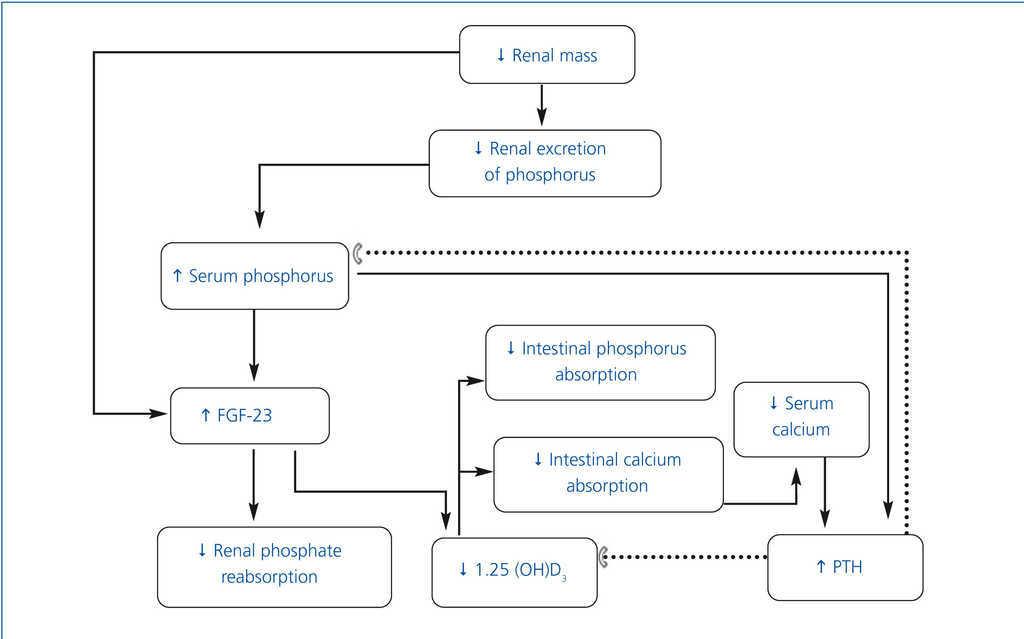
Chronic kidney disease calcium. The association of abnormalities of calcium and phosphate homeostasis with adverse clinical outcomes in chronic kidney disease CKD has generated interest in developing therapeutic strategies to target mineral metabolism early in the course of CKD. Hypocalcemia is quite uncommon in CKD stage 3 and early stage 4 but more often observed in stage 5. Renal failure usually causes calcium.
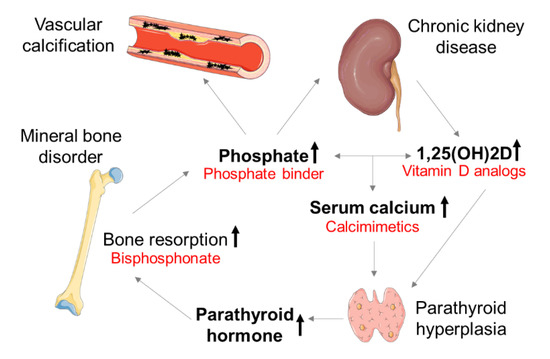
Bicarbonate supplementation preserves renal function in experimental chronic kidney disease CKD but whether the same benefit occurs in humans is unknown. The level of kidney function at which problems start to become apparent is about 40 of normal or an eGFR of 40 mlmin. These imbalances also can cause calcium to deposit in the blood vessels and contribute to heart disease.
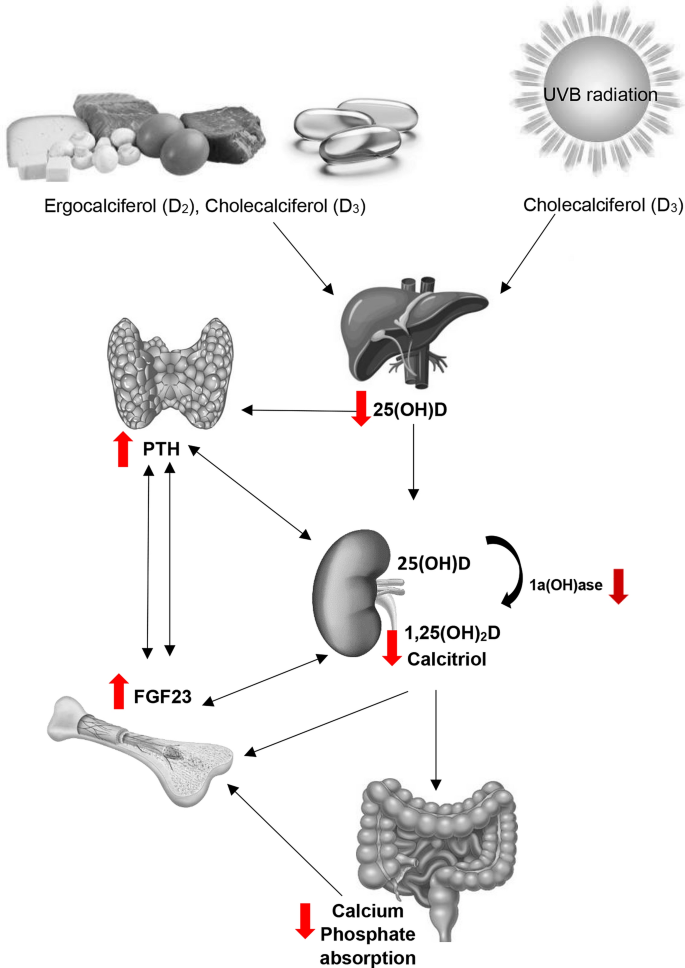
It is often said that patients are treated with calcium for hypocalcemia. The low levels of calcitriol in the body create an imbalance of calcium in the blood. Calcium recommendations for people with chronic kidney disease CKD are very different from those for the general population.
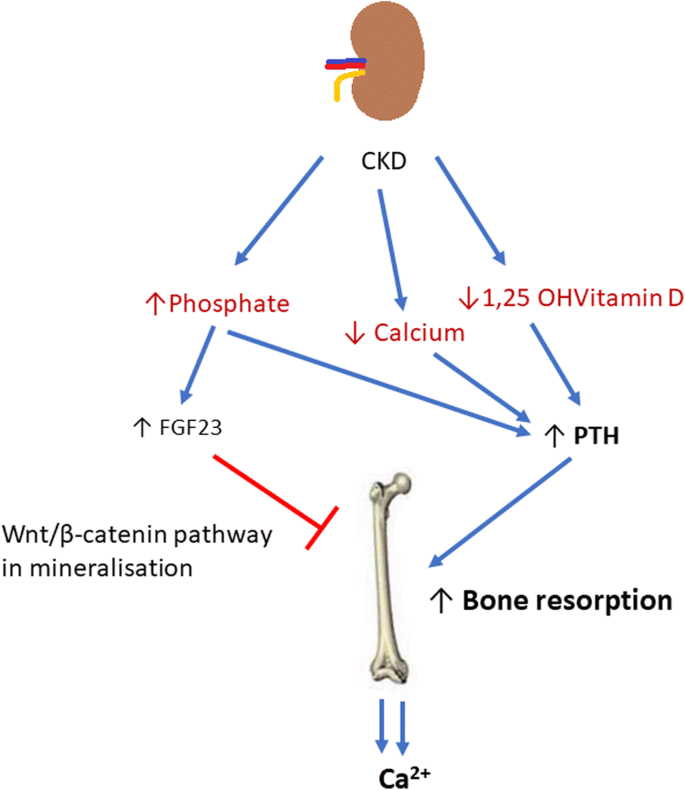
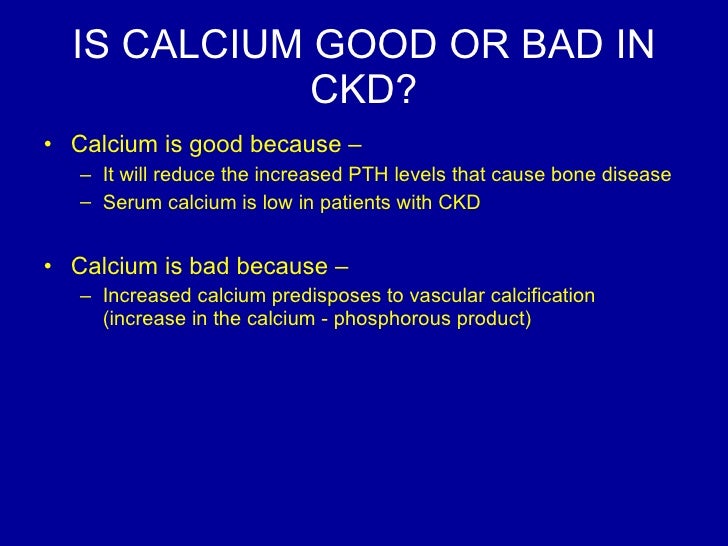
Disorders in chronic kidney disease CKD have been alternately praised and damned. This can then lower serum calcium. Clinical evidence in favor of either attitude has been lacking.
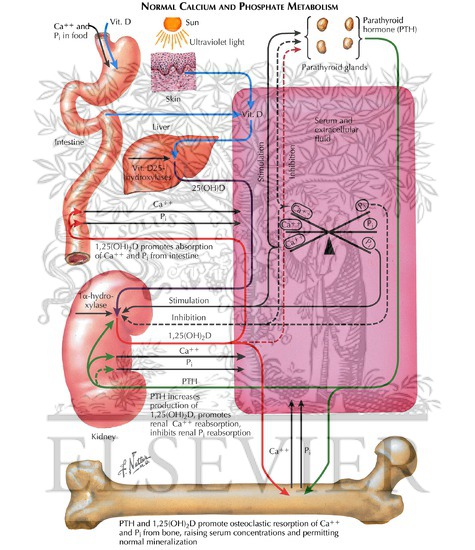
A balanced view of calcium and phosphate homeostasis in chronic kidney disease. Without enough active vitamin D you absorb less calcium from the food you eat so it then becomes low in your blood. As kidney function declines patients may hold onto more calcium and developed high calcium hypercalcemia.
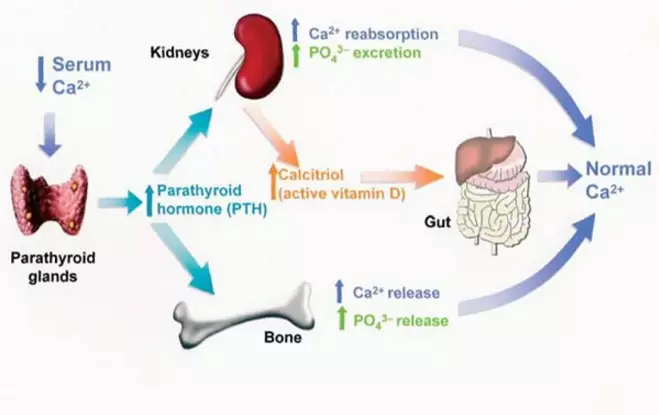
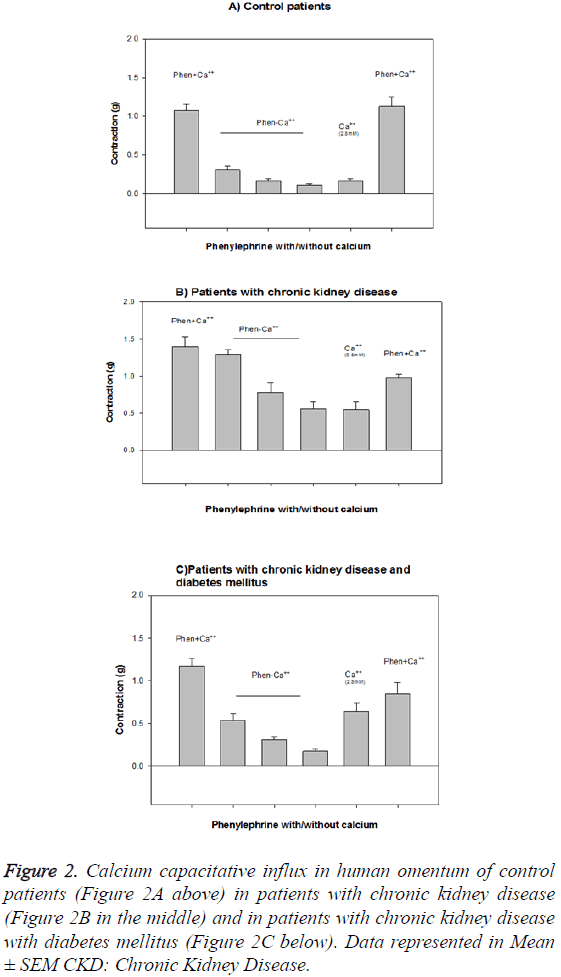
Increases in calcium through diet or supplements cause high positive calcium balance which may put patients at risk for vascular calcification. Calcium homeostasis refers to the hormonal regulation of serum ionized calcium by parathyroid hormone 125-dihydroxyvitamin D and serum ionized calcium itself which together regulate calcium transport at the gut kidney and bone. Hypercalcemia based on serum total calcium total hypercalcemia was observed in 9-22 of dogs 1-3 and in 12-21 45 of cats with CKD.
Calcium supplementation in chronic kidney disease. Calcium and phosphorous usually keep each other in check.
What causes mineral and bone disorder in chronic kidney disease.
For patients with early stage CKD the routine use of calcium in the form of supplements or. This includes calcium from the diet calcium supplements and calcium based phosphorus binders. Hypocalcemia is quite uncommon in CKD stage 3 and early stage 4 but more often observed in stage 5. Bicarbonate supplementation preserves renal function in experimental chronic kidney disease CKD but whether the same benefit occurs in humans is unknown. Chronic kidney disease CKD causes imbalances in bone metabolism and increases the risk of a type of bone disease called renal osteodystrophy. A balanced view of calcium and phosphate homeostasis in chronic kidney disease. This can then lower serum calcium. Calcium supplementation in chronic kidney disease. Also extra phosphorus in the blood of people with CKD may bind to calcium in the blood.
The extra phosphorus pulls. According to the National Kidney Foundation NKF clinical practice guidelines also known as Kidney Disease Outcomes Quality Initiative KDOQI total calcium intake for people with renal disease should not be greater than 2000 mg daily. The level of kidney function at which problems start to become apparent is about 40 of normal or an eGFR of 40 mlmin. How much calcium does a person with kidney disease need. Renal failure usually causes calcium. Calcium recommendations for people with chronic kidney disease CKD are very different from those for the general population. A balanced view of calcium and phosphate homeostasis in chronic kidney disease.

































Post a Comment for "Chronic Kidney Disease Calcium"